Printable Cna Shower Sheets Form in PDF
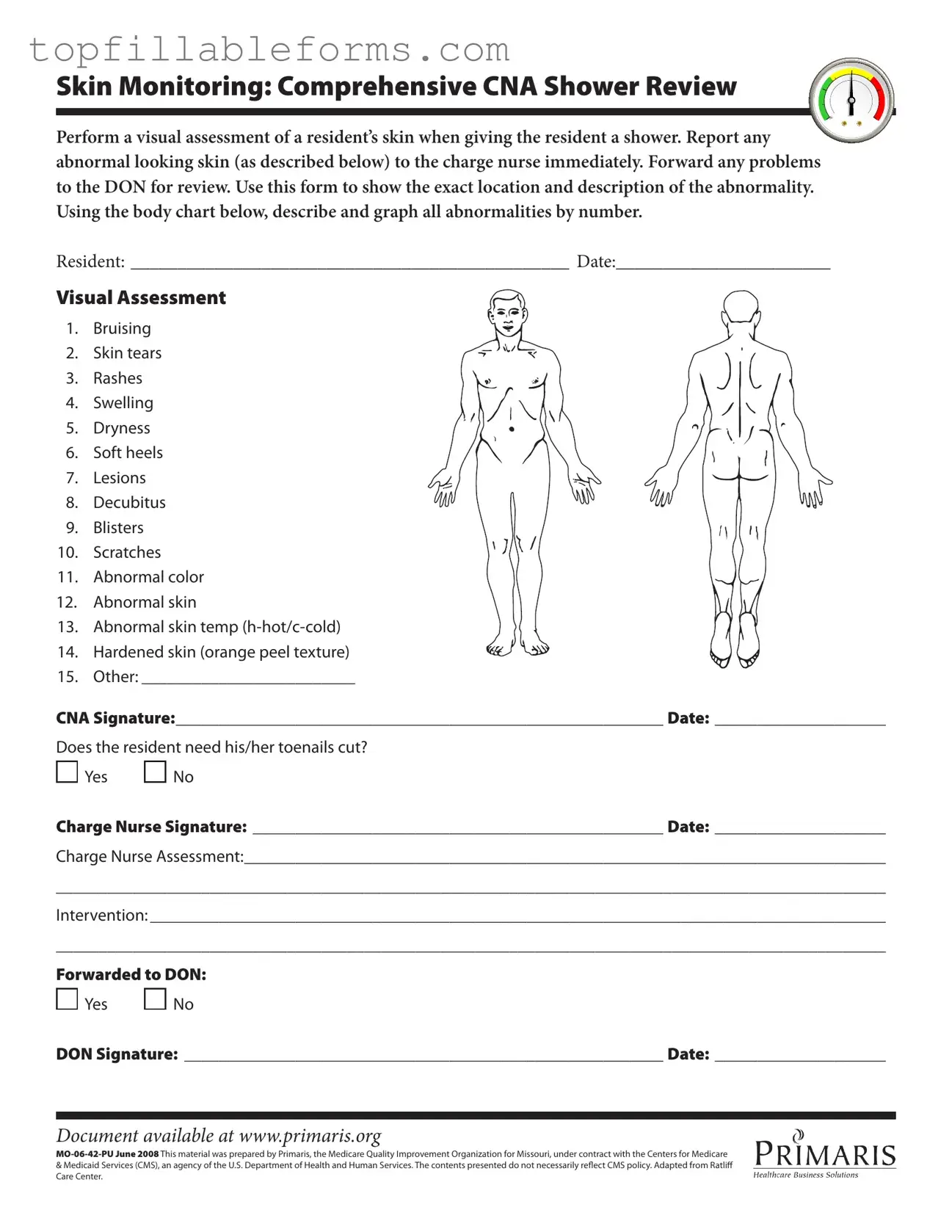
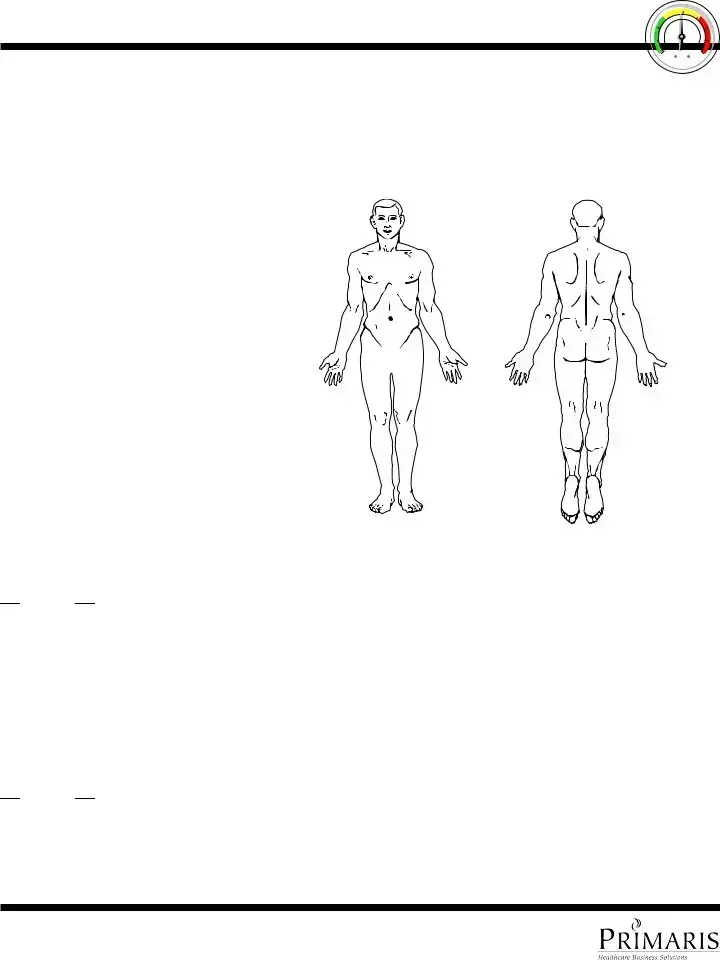
The CNA Shower Sheets form is a vital tool used by certified nursing assistants to document skin assessments during resident showers. This form allows caregivers to note any abnormalities, such as bruising or rashes, ensuring timely communication with nursing staff about potential health concerns. By accurately recording these observations, CNAs play an essential role in maintaining the overall well-being of residents.
Open Cna Shower Sheets Editor Here
Printable Cna Shower Sheets Form in PDF
Open Cna Shower Sheets Editor Here
Finish the form now and be done
Finish your Cna Shower Sheets online by editing, saving, and downloading fast.
Open Cna Shower Sheets Editor Here
or
▼ PDF File

 Yes
Yes 
 No
No
 Yes
Yes 
 No
No