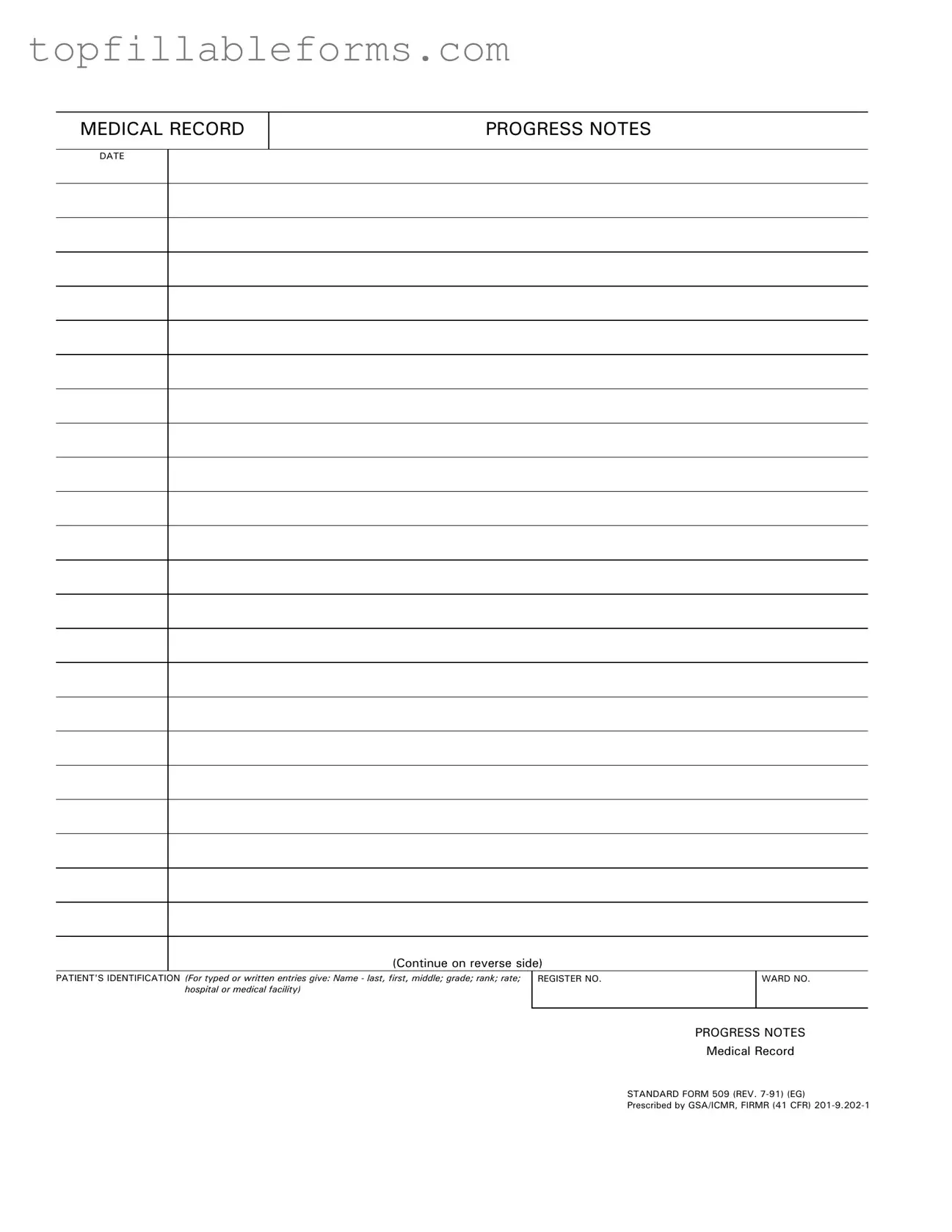
Printable Progress Notes Form in PDF
The Progress Notes form is a standardized document used in medical records to track patient care and treatment over time. It includes essential information such as the patient's identification, date, and details of their progress. This form plays a crucial role in ensuring continuity of care and effective communication among healthcare providers.
Open Progress Notes Editor Here
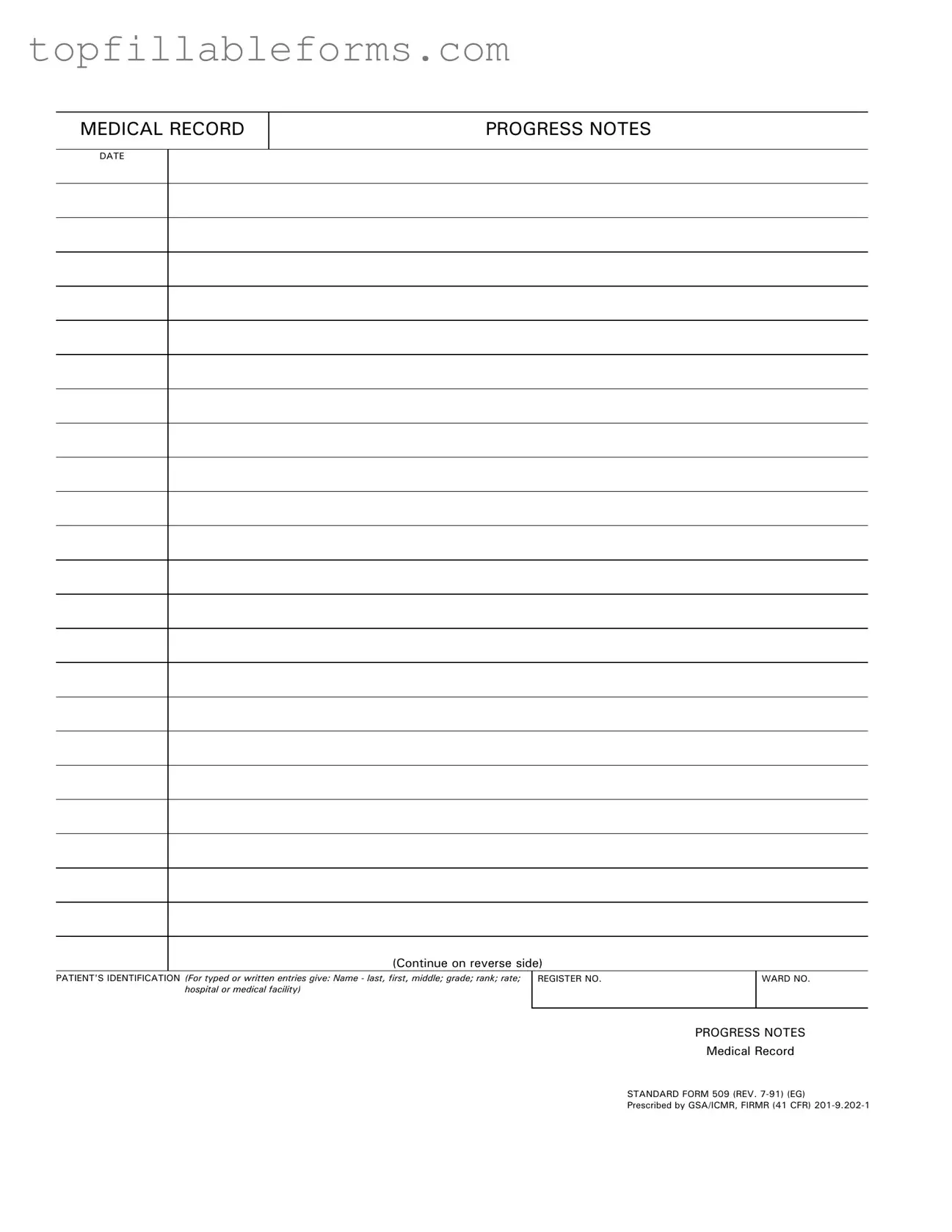
Printable Progress Notes Form in PDF
Open Progress Notes Editor Here
Finish the form now and be done
Finish your Progress Notes online by editing, saving, and downloading fast.
Open Progress Notes Editor Here
or
▼ PDF File