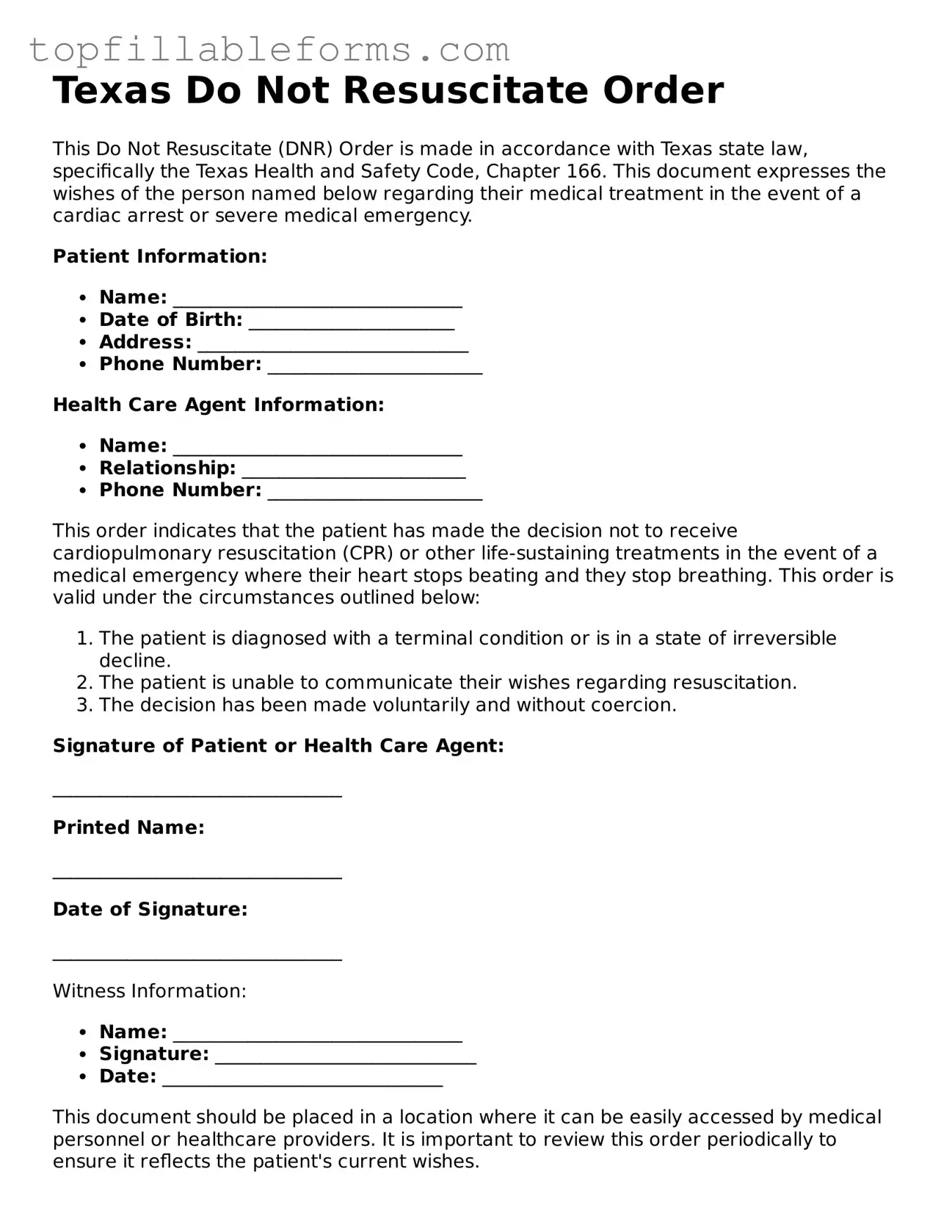
Attorney-Verified Do Not Resuscitate Order Template for Texas
A Texas Do Not Resuscitate Order (DNR) form is a legal document that allows individuals to express their wishes regarding resuscitation efforts in the event of a medical emergency. This form ensures that healthcare providers understand a person's desire to forgo life-saving measures. Understanding the implications of a DNR is essential for both patients and their families.
Open Do Not Resuscitate Order Editor Here
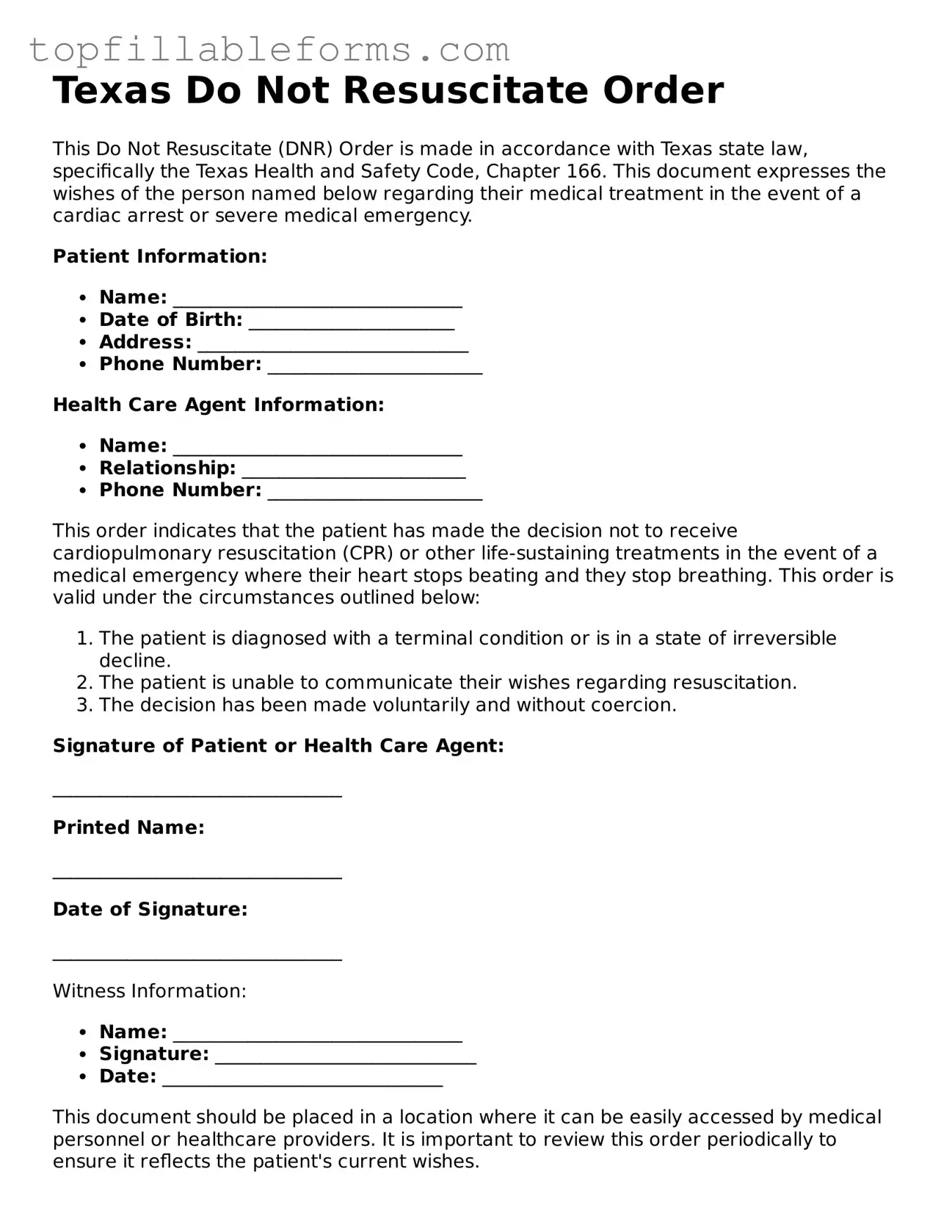
Attorney-Verified Do Not Resuscitate Order Template for Texas
Open Do Not Resuscitate Order Editor Here
Finish the form now and be done
Finish your Do Not Resuscitate Order online by editing, saving, and downloading fast.
Open Do Not Resuscitate Order Editor Here
or
▼ PDF File